Before America’s first stay-at-home orders, before school and business closings, before overwhelmed hospitals and the confirmation that the world is facing a deadly pandemic, scientists at the University of Pittsburgh were hard at work on research that could prove key to stopping the COVID-19 pandemic.
The virus arrived at Pitt in mid-February. It came not in an infected person, but in a vial, stuffed inside a plastic bag, sealed inside a cylinder, packed in dry ice, encased in Styrofoam, and sheathed in cardboard.
The highly secure delivery was made to the Biosafety Level 3 laboratory in the University of Pittsburgh’s Center for Vaccine Research (CVR), where Paul Duprex, the center’s director, and colleagues Amy Hartman, William Klimstra, Anita McElroy and Doug Reed were poised to begin work on interventions and vaccines. They had met with safety colleagues just 10 days before to launch their first COVID-19 task force, which has met every week since.
Pitt was one of the first institutions in the country to receive the virus directly from the Centers for Disease Control and Prevention—and it is specially equipped to take it on. With support from the National Institute of Allergy and Infectious Diseases within the National Institutes of Health, the CVR’s facilities are specifically designed to handle this kind of high-stakes work, and its staff have years of experience working in biocontainment. Pitt also has a legacy of tackling vaccine challenges, including, of course, Jonas Salk’s work on the polio vaccine in the 1950s.
The CVR’s focus quickly shifted to combating the virus. By mid-March, Duprex, the Jonas Salk Chair for Vaccine Research, and his team had earned further support. They were part of a $4.9 million grant to develop and test a COVID-19 vaccine as members of a three-way partnership with Institut Pasteur in Paris and Themis Bioscience, a biotech company based in Vienna. Awarded by the Coalition for Epidemic Preparedness Innovations, the grant was a big vote of confidence from an organization known as a leader in vaccine development.
So, how do scientists quickly develop a vaccine amid an active and evolving pandemic?
“We can use what we know about viruses and look for the weak points,” says Duprex.
The researchers’ efforts are zeroed in on perhaps the most visually notable component of the pathogen as it’s depicted in computer-generated renderings seen so often in the press: the parts that look like little red knobs sticking out of a gray sphere.
These are spike proteins, a feature of all coronaviruses. Research has shown that they can induce immunity by prompting the generation of antibodies, which fight the virus and build a person’s resistance to future infection.
To create a vaccine using spike proteins, Duprex has applied his expertise in measles, the “most infectious human virus on earth,” he says. A safe and effective measles vaccine already exists and has been successfully adapted to tackle other viruses. Duprex and his colleagues are genetically engineering the measles vaccine to include minuscule pieces of novel coronavirus spike proteins. The intended result: a vaccine candidate that may provide protection from SARS-CoV-2, the virus that causes COVID-19.
Testing the candidate vaccine in animal models is already underway in Paris and Pittsburgh. If all goes well, two Phase 1 clinical trials with 50 to 100 patients are expected to begin in Europe this summer. Should it eventually be approved for widespread use, the team is preparing to ensure that millions of doses of the vaccine can quickly reach the public as the consortium begins to work with the Serum Institute of India to manufacture the vaccine on an industrial scale.
Meanwhile, the CVR team continues to expand its COVID-19 footprint as it moves rapidly into other potential treatment options. Since 2012, Duprex’s colleague Klimstra has been working with SAb Biotherapeutics, a company based in South Dakota, to develop antibodies that fight certain viral infections. Now they are using a creative approach to create SARS-CoV-2 antibodies from spike proteins injected into specially generated cows that are capable of producing large numbers of human antibodies indistinguishable from our own. Klimstra’s team is already several steps into testing the efficacy of these antibodies against the coronavirus by using the animal models the CVR task force has developed to test the measles-COVID-19 candidate vaccine.
“Everything moves so quickly,” he says. “The company is working with the FDA and they are hoping to begin human clinical trials sometime in mid-July. In all the years we have worked with them I’ve seen nothing move so fast.”
“Timelines are ridiculously rapid by vaccine development standards,” agrees Duprex, but they still aren’t speedy enough for a world that needs a vaccine or therapeutic tomorrow. Even so, the CVR scientists acknowledge that researchers today have an advantage over Salk, who spent six years on the polio vaccine: “We can manipulate, we can alter the genetics, the compositions of these viruses in ways that Dr. Salk could only have dreamed,” Duprex says.
The CVR team is making significant progress in both antibody therapeutics and vaccine candidates. There are hundreds of approaches and scores of vaccines in development around the world. However, it isn’t about who gets there first, says Duprex. It’s about helping to find a solution that will save lives. There’s a moral imperative to contribute to the effort to stem the pandemic, guided by the fact that Pitt’s CVR researchers have been entrusted with the facilities needed to get the work done.
And that’s exactly what they will do.
 Additional Efforts
Additional Efforts
The researchers at the CVR aren’t the only ones at Pitt working to address the pandemic. In late March, Pitt’s Clinical and Translational Science Institute (CTSI) launched the COVID-19 Pilot Grant Program to help fund pandemic-related research. A total of 157 projects were submitted for grant consideration, representing 590 unique investigators from 14 different Pitt schools and more than 90 Pitt departments, divisions, centers and institutes. Collaboration abounds: Researchers are working with 46 different universities, as well as 11 companies and 15 nonprofit governmental organizations.
 There is also another vaccine study unfolding at the University, this one led by Pitt School of Medicine’s Louis Falo, professor and chair of dermatology, and Andrea Gambotto, associate professor of surgery. Though unrelated to Duprex and the CVR, their efforts also involve the descriptively named spike protein for its immunity inducing capabilities. It’s an approach Gambotto knows well, having extensively studied SARS and MERS, two viruses closely related to the virus that causes COVID-19.
There is also another vaccine study unfolding at the University, this one led by Pitt School of Medicine’s Louis Falo, professor and chair of dermatology, and Andrea Gambotto, associate professor of surgery. Though unrelated to Duprex and the CVR, their efforts also involve the descriptively named spike protein for its immunity inducing capabilities. It’s an approach Gambotto knows well, having extensively studied SARS and MERS, two viruses closely related to the virus that causes COVID-19.
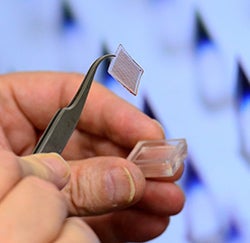
 Falo and Gambotto’s research paper, released in early April by EBioMedicine, part of The Lancet’s family of journals, was the first peer-reviewed COVID-19 vaccine candidate study to be published. In it, they detail how their team developed lab-made pieces of the spike protein—tiny, synthetic subunits of the virus—to create a potential vaccine. To increase potency and ease of administration, they also designed a novel delivery method—painless, Band-Aid-like patches for the skin.
Falo and Gambotto’s research paper, released in early April by EBioMedicine, part of The Lancet’s family of journals, was the first peer-reviewed COVID-19 vaccine candidate study to be published. In it, they detail how their team developed lab-made pieces of the spike protein—tiny, synthetic subunits of the virus—to create a potential vaccine. To increase potency and ease of administration, they also designed a novel delivery method—painless, Band-Aid-like patches for the skin.
When tested in mice, PittCoVacc (short for Pittsburgh Coronavirus Vaccine) produced antibodies sufficient for neutralizing the virus. They hope to start a Phase 1 clinical trial with a small group of patients soon. Meanwhile, with help from a CTSI grant, they are also working to develop a mouse model that would be ideal for testing various aspects of COVID-19 vaccine design in the future.
Breakthroughs in the Making
Nervy Work
Major damage to nerves outside of the brain or spinal cord can cause big problems. The only treatment option is grafting a healthy nerve from another part of the body onto the injury, but the procedure has limitations. Kacey Marra, a professor in Pitt’s departments of plastic surgery and bioengineering, and her team are working on an alternative: a biodegradable polymer tube that releases a nerve growth-promoting protein. When implanted in a nonhuman primate model, the device helped rebuild a damaged nerve and restored nearly 80 percent of its function. The research, published in Science Translational Medicine, could one day aid some of the 600,000 Americans who sustain nerve injuries annually.
Septic Statistics
Whether treating patients in rural Uganda, Thailand or Pittsburgh, Kristina Rudd regularly saw cases of sepsis, a life-threatening immune response to infection. Today, the Pitt professor of critical care medicine is researching the problem. “How can we know if we’re making progress if we don’t know the size of the problem?” she asked. Rudd’s team and colleagues at the University of Washington recently conducted a global analysis, published in The Lancet, revealing that sepsis is associated with 1 in 5 deaths worldwide, double previous estimates. The authors suggest that strengthening public health infrastructure, improving vaccine access and fighting antimicrobial resistance may help combat these odds.
The Power of Protest
When protesters target major corporations, what approach is most likely to inspire the company to meet their demands? According to a study by Tarun Banerjee, a Pitt sociology professor, and graduate student Benjamin Case, damaging a company’s bottom line—not its reputation or media coverage—makes the biggest difference. In evaluating the disruptive impacts social movements had on large U.S corporations from 2005-2009, they found that protests were most successful when they led to negative valuations of companies’ share prices, while tactics that generated large amounts of or negative media coverage were usually not enough to bring about change.
Cover image: Paul Duprex
This article appears in the Summer 2020 edition of Pitt Magazine.