At a clinic in the coastal city of Recife, Brazil, a pediatric neurologist pores over the day’s case files. Vanessa Van der Linden has never seen anything like this before. Babies born with microcephaly—abnormally tiny heads and disordered brains—are suddenly appearing in her maternity ward. All of the area’s hospitals combined see no more than 10 cases a year. Today alone, she has diagnosed three.
Worry swells in the doctor’s chest. She picks up her cell phone and calls her mother, another pediatric neurologist working in a nearby hospital. “Mommy,” she says in Portuguese. “Há algo errado.” There is something wrong.
Soon, physicians across northeastern Brazil report similar surges of microcephaly cases rising like a tide from the region’s poorest neighborhoods. The search is on to find the cause behind the crisis.
About 10 months before that moment in the clinic, at the start of Brazil’s equatorial rainy season in late 2014, doctors were grappling with a different kind of medical mystery. Reports emerged of an unidentified but seemingly benign illness in the country’s northeast. Its symptoms were graciously mild. Most patients complained of a raised, red skin rash, joint aches, and eye irritation. Some had low fevers. The discomfort lasted only a few days and rarely required treatment beyond a pain reliever. No one guessed that it was the first, early sign of new trouble.
Dengue fever, a mosquito-borne viral disease well known to Brazil, also causes fever, rash, and joint pain—but the match wasn’t exact. Dengue, which belongs to the flavivirus genus, is more debilitating. Some infections can generate severe and deadly symptoms, causing hemorrhagic bleeding and joint pain so crushingly intense that a common nickname for the virus is “break-bone fever.”
In the absence of other credible theories and with conflicting lab data, many experts, including those at the Brazilian Ministry of Health, hypothesized that the unknown illness was dengue, but in a mild form. By March 2015, more than 7,000 cases had been reported.
Pitt researcher Ernesto T.A. Marques closely followed news of the so-called “dengue light” cases. An associate professor of infectious diseases and microbiology in Pitt’s Graduate School of Public Health, Marques splits his time between Pittsburgh and Recife.
“I have, let’s say, a job-related double personality,” Marques notes with a laugh. His attention often shifts between two different worlds simultaneously—the United States and Brazil; the classroom and the lab; English and Portuguese. But the mystery around the unidentified, enigmatic disease gave the researcher’s focus yet another target.
Marques grew up in Recife, the grandson of a pharmacist. His father ran the business. As a boy, dark-eyed and curious, Marques would watch as neighbors came to the drugstore for help with what ailed them.
He was still in high school when he decided to become a doctor, but it wasn’t until he reached medical school at Universidade Federal de Pernambuco in Recife that he chose the research track. The detective work of medical research excited him. He loved to explore a problem from all of its angles, delving into its most complex components to better understand its whole.
“I was curious,” he says. “You’re learning these very broad medical theories, and I wanted to know, how did people figure that out? And how could it be done a little better?”
Marques was drawn to translational research, to science that could be turned into solutions to major health problems. The study of human immunology, or the way the body’s immune system responds to different diseases, became the lens through which he could investigate viruses and their potential preventative vaccines—particularly those that plague Brazil. He felt something of a duty to serve people in his home country, just as his father and grandfather did.
“Others may have the resources and opportunity to respond to Brazilians’ issues, but they don’t have the actual experience of the reality that the patients live,” Marques says. “I think I can see with the eyes of people who actually have to deal with the problems.”
 One problem that Marques saw troubling Brazil was dengue. He zeroed in on the disease, among others, while earning a PhD in pharmacology from Johns Hopkins University. He became a dengue expert, developing new ways to detect its most severe manifestation and inventing a prognostic tool that helps doctors predict the health outcomes of dengue-infected patients. But as he finished his postdoctoral work, he knew that to best study dengue and other mosquito-borne diseases, he had to be close to the people most affected.
One problem that Marques saw troubling Brazil was dengue. He zeroed in on the disease, among others, while earning a PhD in pharmacology from Johns Hopkins University. He became a dengue expert, developing new ways to detect its most severe manifestation and inventing a prognostic tool that helps doctors predict the health outcomes of dengue-infected patients. But as he finished his postdoctoral work, he knew that to best study dengue and other mosquito-borne diseases, he had to be close to the people most affected.
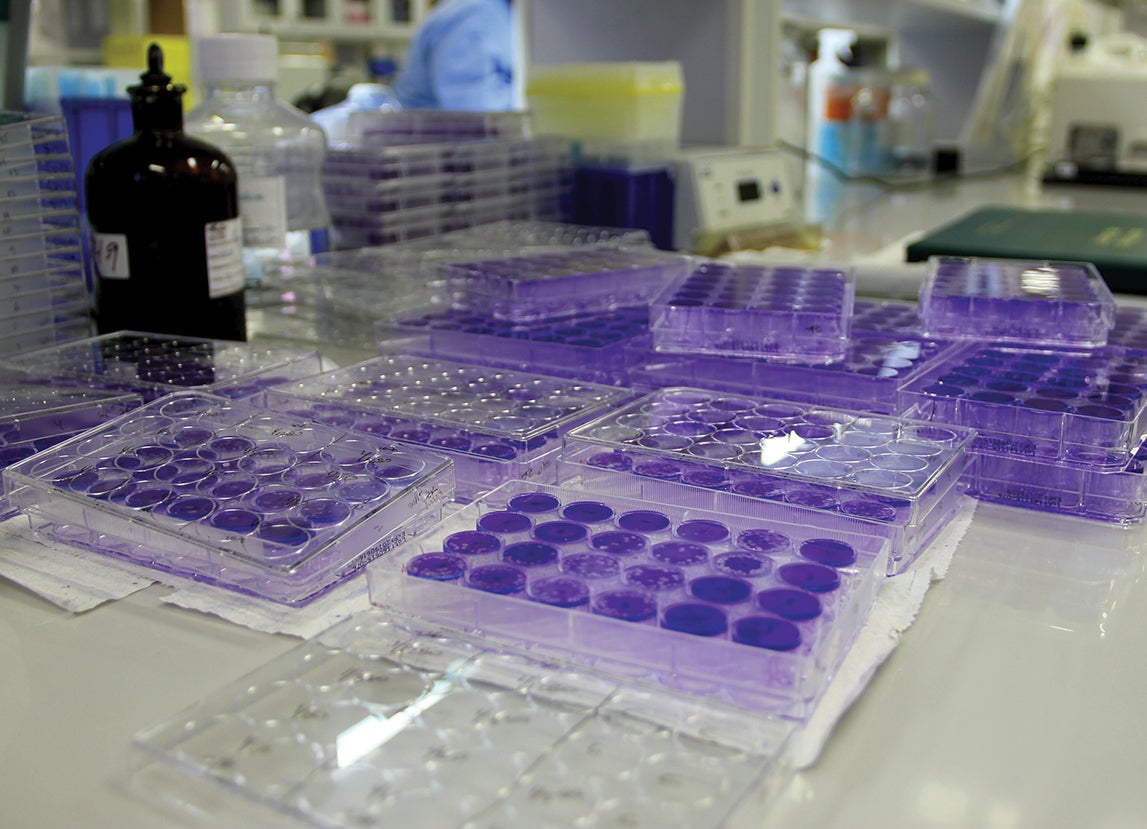
So there, in the sprawling, beach-lined city where he grew up, Marques built a collaborative lab with one of South America’s most prestigious medical research institutions, Fundação Oswaldo Cruz (FIOCRUZ) Institute. In 2009, when he accepted a professorship at Pitt, the Recife laboratory became one of three international research sites partnered with the University of Pittsburgh Graduate School of Public Health. Marques serves as a liaison between Pitt and FIOCRUZ, connecting scientists from both institutions.
The nature of the research unfolding in the Recife lab is similar to what’s taking place at Pitt’s Center for Vaccine Research, where Marques is also affiliated. It’s translational and incremental, with each study moving researchers closer to unpacking the mysteries of infectious diseases in an effort to better identify, treat, and stop them from spreading.
But viruses are particularly tricky subjects. Experience has taught Marques that they are capable of unexpected behavior, and that studying them can be like trying to stare steadily at a moving target. The reach of a virus and its effect on a human host hangs on a multitude of factors including the history of community exposure to similar viruses. Big and small changes in things like environment, human behavior, immune responses, or the virus’s genetic composition can alter its scope, allowing it to jump countries or continents, spreading widely or receding quietly. Researchers often aren’t even aware of a virus’s full capability until it is demonstrated by an outbreak. But buried within the structure and behavior of a virus, there are clues about how best to diagnose, treat, and even stop it.
At the time of the appearance of the mystery illness, Marques and his lab were focused on a collection of studies investigating dengue immunology. Immersed in this research, he eyed the “dengue light” outbreak closely, though he remained relatively unconcerned. Whatever it was, it didn’t appear to be dangerous. “That,” he says, “was the assumption.”
As 2015 unfolded in Brazil, a meeting was called between Brazilian clinicians and infectious disease specialists at FIOCRUZ. The group’s aim was to determine through laboratory testing just what was making people sick in the northeast.
As the meeting convened, Marques participated from a continent away. From his office on the ninth floor of Pitt’s Biomedical Science Tower 3, he engaged with the proceedings through a video feed on his computer. He listened as the group combed through a list of viral possibilities both obscure and common. There was dengue, of course, but also chikungunya, Mayaro, and Zika, a little-known flavivirus last seen in early 2014 on the tiny islands of French Polynesia.
“To be honest,” says Marques, “it was not my favorite on the list.” He felt dengue was more likely because Zika had never been seen in Brazil before. But his Brazilian colleague Carlos Brito argued that Zika’s symptoms matched those currently reported. He also pointed to an apparent uptick across the region of a neurological condition in adults called Guillain-Barre syndrome. Data from French Polynesia’s Zika outbreak revealed a similar increase.
The meeting ended with an agreement to put Zika on the shortlist of culprit viruses. Marques’s lab was already testing “dengue light” patient samples for dengue and another virus. He signed on to test samples for Zika, too. While other scientists searched for evidence of a Zika outbreak in Brazil, the Pitt researcher’s lab had a narrower focus—to see whether there was evidence that those with recently diagnosed Guillain-Barre had also been infected with the Zika virus.
Within two months, colleagues confirmed that Zika was in Brazil. Soon after, the Pitt/FIOCRUZ lab released its findings, too: the virus’s antibodies were indeed present in the blood of Guillain-Barre patients tested—and, for the first time, it was identified in their cerebrospinal fluid as well. That suggested, worryingly, that in certain cases Zika might selectively target the body’s nervous system.
One thing was clear—the virus traveled across time and vast territory to reach South America, likely through global travel and trade. It was first identified in 1947 in a rhesus monkey living in a tropical forest in southern Uganda. Researchers named the new virus after the forest where it was discovered. Zika, in the area’s native Lugandan language, means “overgrown.”
The first documented human cases of the virus appeared in East Africa in 1952, transmitted, just as it was to monkeys, by the bite of an infected aedes aegypti mosquito. Over the subsequent decades, because of its mild symptoms, the virus didn’t inspire much alarm or research. Prior to 2007, only 14 cases of Zika were recorded throughout the world. There had never been a known outbreak of the scale now suggested in Brazil.
But it appeared that Zika had begun to live up to its “overgrown” name.
Back in Pittsburgh, Marques took the news of Zika’s emergence to Donald Burke, dean of Pitt’s Graduate School of Public Health, associate vice chancellor for global health, and UPMC-Jonas Salk Chair in Global Health. Burke, a world-renowned expert in emerging diseases, has an intimate understanding of viruses and outbreaks. He was already familiar with Zika, having written the definitive textbook description of the virus more than a decade ago. And, like Marques, he knew the benefit of vigilance.
Although the virus appeared to be a benign infection of adults, the two men drafted an email to a former colleague of Burke’s working in the Biological Threats Defense department in the White House.
“If Zika is in fact spreading in Brazil,” wrote Burke, “it is of concern for several reasons. 1. It will cause confusion about what is dengue and what is Zika, and what will be vaccine preventable. 2. It could spread more widely in the Americas. 3. There may be surprising interactions of Zika and dengue.”
“I think it is important that surveillance for Zika be implemented … as soon as possible,” Marques wrote. “Much needs to be done.”
The note, written in spring 2015, did not provoke immediate governmental action. Though Zika was slowly revealing its capabilities, the virus wouldn’t become an international concern until the outbreak took a strange and alarming turn.
The first suspicious case of microcephaly observed by pediatric neurologist Vanessa Van der Linden appeared in late August 2015. The baby’s mother was healthy. She didn’t report exposure to any of the common microcephaly causes during her pregnancy—no measles, toxoplasmosis, drugs, or alcohol. She did, however, remember having a light red skin rash during her first trimester. It lasted only one day; she thought little of it.
 By late September, Van der Linden and other physicians had seen many cases like the first: healthy mothers who may have had a viral infection during pregnancy, and their severely disordered babies. Troubled, she shared her findings with colleagues including her old med school classmate, Ernesto Marques.
By late September, Van der Linden and other physicians had seen many cases like the first: healthy mothers who may have had a viral infection during pregnancy, and their severely disordered babies. Troubled, she shared her findings with colleagues including her old med school classmate, Ernesto Marques.
He shared her concern, and so did their colleague, physician Carlos Brito, who again pointed to Zika. “He made the connection that the mothers would have been in their first trimesters at the peak of the Zika outbreak,” Marques explains. And the fact that the virus could infiltrate the central nervous system of some adults provided an additional clue.
Did these babies contract the virus from their mothers while in the womb, the infection disrupting their development? The Pitt/FIOCRUZ lab began testing to find out.
Thirty newborns with microcephaly were tested—and the results showed that all of them once had Zika. Marques, along with fellow researchers Marli Tenorio Cordeiro, Lindomar J. Pena, Carlos Brito, and Laura H. Gil, published their findings in the medical journal the Lancet, becoming the first researchers to provide “strong evidence that the microcephaly was a consequence of Zika virus infection.”
Even before the research was published, Marques was working on the next set of questions in urgent need of answers. Zika no longer presented as the benign virus it appeared to be 70 years ago; it had revealed itself to be complex and capable of harm.
Last fall, despite the continued spread of the virus, the World Health Organization declared an end to Zika’s classification as a “Public Health Emergency of International Concern.”
But, says Marques, it is hard to define a threat that is still coming into focus.
“The hope that Zika is gone,” says Marques, “is not quite right.”
Much about the virus remains unknown and—given Zika’s unexpected capabilities to cause serious harm in some cases—research has more to tell us about viral diseases and how to stop them.
“All of the easy questions have been answered,” says Marques about Zika. “Now, we’re working on the difficult ones.”
One line of inquiry Marques is exploring is why Zika infections can be devastating to some, while others are unaffected. Since arriving in South America, the virus has spread to at least 84 countries, including the United States, but no other population has the same high number of Zika-affected babies as Brazil. Even there, not every infected pregnant woman gives birth to a child with a Zika-related disorder. Why?
Marques’s recent lab data have shown that the presence of dengue antibodies can make a Zika infection more severe, both for the initial host and for a fetus that may contract the virus through a mother’s placenta. The process is called antibody-dependent enhancement. If, as Marques suspects, enhancement is playing a role in Zika’s seemingly selective effect, that piece of information will play a vital role in the development of a safe and effective vaccine, while also helping infectious disease specialists to anticipate and prevent new viral epidemics.
And that’s at the heart of most infectious disease specialists’ mission—to dig ever deeper, excavating unknowns in pursuit of either stopping diseases before they emerge into deadly epidemics, or stemming their impact.
At the Graduate School of Public Health and Pitt’s Center for Vaccine Research, building a global network is a vital component of this work. Labs like the one in Recife—positioned at the frontlines of potential outbreaks—can offer researchers a head start in tackling the next emergency. When you’re studying viruses, which are covert and often fast moving, there’s a real advantage to being even one step ahead of the curve.
 Recently, Marques and his team developed a new, faster, and better way to diagnose Zika, potentially making response to the outbreak and the development of vaccines that much easier. But if there’s any chance of preventing the world’s next Zika epidemic, the research must be done now.
Recently, Marques and his team developed a new, faster, and better way to diagnose Zika, potentially making response to the outbreak and the development of vaccines that much easier. But if there’s any chance of preventing the world’s next Zika epidemic, the research must be done now.
Pitt’s Graduate School of Public Health is seizing the momentum. Marques and Burke founded Cura Zika, an international research alliance that targets the epidemic through continued collaboration between researchers at Pitt and FIOCRUZ.
“We wanted to do this as a Brazil and U.S. cooperation,” says Burke, who serves as the program director alongside Marques, the scientific director. “This is about their epidemic. The question was, what could we do to help?”
The Cura Zika foundation provides funding for studies across both institutions with efforts that range from research to better understand Zika’s impact on mothers’ placentas to the engineering and evaluation of a Zika vaccine. In recent months, the work of Cura Zika has been highlighted in the New York Times and other media. In 2017, Celina Turchi—a FIOCRUZ epidemiologist who is a scientific advisor with Cura Zika, a close collaborator with Marques, and the senior investigator in the case-control study that linked Zika to microcephaly—was named one of Time magazine’s most influential people of the year.
Yet, much about the virus is still unknown. “There are potentially decades more work for us,” says Marques, whose pace remains urgent.
These days the Pitt researcher spends most of his time working in his lab, on airplanes, and behind the blinking cursor of journal articles in the making. But no matter where he is, Marques is likely thinking of Zika and Brazil, sifting the possibilities, the knowns and unknowns.
This article appeared in the Summer 2017 issue of Pitt Magazine.





