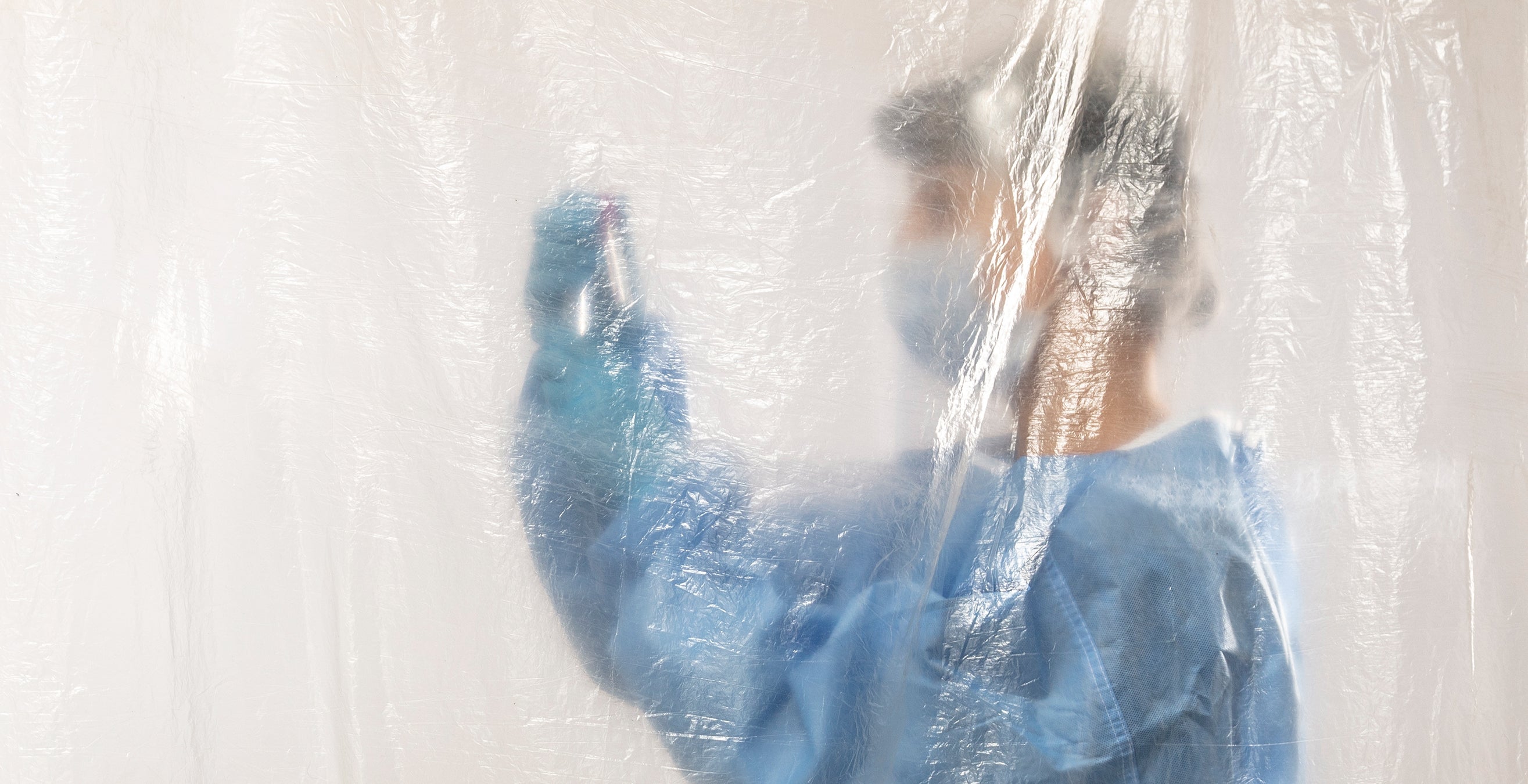
Underneath Meghan Hodgson’s multiple face masks and face shield, tears threatened to overtake her. It was March 2020, and the registered nurse was working a regular night shift in the emergency room at her suburban New Jersey community hospital. But for Hodgson (NURS ’03), nothing about this night was normal.
A mysterious flu-like illness was swiftly and covertly making itself at home in communities everywhere, and more and more people were becoming ill—people like “Jane,” a 52-year-old woman with Down syndrome, who had come into Hodgson’s ER seeking care. Masked and isolated in a sterile room, with no visitors allowed, Jane lay on her back, eyes closed. Unmoving and alone.
 In the year since the emergence of the coronavirus pandemic, Jane was just one of more than 100 million people afflicted with the life-threatening virus. COVID-19 has posed challenges to nearly every facet of life; perhaps no one is more attuned to these challenges than the health care providers, like Hodgson, and the researchers trying to rein in a virus run rampant.
In the year since the emergence of the coronavirus pandemic, Jane was just one of more than 100 million people afflicted with the life-threatening virus. COVID-19 has posed challenges to nearly every facet of life; perhaps no one is more attuned to these challenges than the health care providers, like Hodgson, and the researchers trying to rein in a virus run rampant.
“It sounds cliché, but it’s everywhere, and it’s not going anywhere,” says Christopher Seymour, an associate professor of critical care medicine and emergency medicine in Pitt’s School of Medicine and an intensivist at UPMC Mercy. He adds that vaccines, though necessary, won’t eradicate the virus. “In time,” he explains, “COVID-19 will become this long, smoldering cause of illness, just like many of the others we take care of in the ICU.”
With that prognosis, it will take a combined effort between preventatives (including vaccines) and treatments (from repurposed to newly developed drugs) to effectively control the pandemic. The University of Pittsburgh is playing a critical role in that effort.
“In terms of the majority of vaccines and therapeutics that actually make it into the marketplace, their initial studies are done in a university environment as basic science,” explains William Klimstra, an associate professor of immunology at Pitt. In other words, drugs of tomorrow that could help treat patients like Jane typically get their start in academic research labs.
For Hodgson, tomorrow can’t come soon enough. Remembering those long ER nights with Jane in March 2020, Hodgson hadn’t felt so overwhelmed since her first year out of nursing school. And for the 18-year nursing veteran and mother of five girls (including triplets), that was saying something. “The first year of nursing was very trying, exhausting,” she remembers. “You question everything you do.” COVID-19 has left her questioning everything again.
Early in the pandemic, Hodgson and her colleagues privately referred to what they witnessed in the ER as the “zombie apocalypse.” Many patients—disoriented as a result of low blood oxygen levels that can accompany COVID-19—would clumsily remove their nasal cannulas, climb out of bed and try to pull out their IVs, which only exacerbated their symptoms. In the midst of performing various duties, nurses, including Hodgson, flew from room to room to resettle their patients.
Hodgson’s shift in March 2020 continued as the previous one did: Every hour, she attended to her patients like Jane, whom she tried to keep comfortable, stroking her hair, talking to her. There was no response. Following the do-not-resuscitate order from the patient’s family, she watched as the bedside monitor reflected Jane’s worsening pulse and oxygen levels. Her organs were slowly shutting down. By the end of Hodgson’s shift, the nurse wondered whether Jane would survive the next 12 hours.
Throughout 2020 and into 2021, as health care workers like Hodgson contended with a novel illness, there was often only so much they could do for their patients—what Seymour refers to as “normal supportive care, no advanced therapies.”
 At Pitt, where there is a wealth of experts interested in infectious diseases, researchers are doing their part to fill the treatment void, through clinical studies of preexisting drugs that may combat the virus as well as the discovery and development of novel therapeutics. Both approaches are necessary because researchers and clinicians point out that there will be no one “magic bullet” to treat COVID-19—but rather, as Seymour says, a combination of drug treatments, which will be determined by the symptoms and medical history of each patient.
At Pitt, where there is a wealth of experts interested in infectious diseases, researchers are doing their part to fill the treatment void, through clinical studies of preexisting drugs that may combat the virus as well as the discovery and development of novel therapeutics. Both approaches are necessary because researchers and clinicians point out that there will be no one “magic bullet” to treat COVID-19—but rather, as Seymour says, a combination of drug treatments, which will be determined by the symptoms and medical history of each patient.
The pursuit of novel therapeutics involving antibodies may have far-reaching, life-saving implications. Antibodies are proteins that are naturally produced in the body. They recognize a pathogen as a foreign invader and block its entry into a person’s cells; for example, an antibody for COVID-19 would ideally thwart the virus from spreading in the body or stop the disease’s progression altogether without harming healthy cells. Once researchers identify the antibodies best suited to fight COVID-19, the proteins could then be mass-produced for widespread use as a drug.
Multiple COVID-19 antibody treatments are in development by Pitt-affiliated research groups—including those led by Klimstra, Dimiter Dimitrov and Yi Shi, all of Pitt’s School of Medicine.
Medical professionals understand the significance of the research, with one caveat: “The problem that we’re facing today,” Seymour says, “is that that science takes time; novel therapeutics take time to develop and then test.”
Fortunately, for Klimstra, Dimitrov and Shi—with decades of training and scientific investigation already in their arsenals—they had the flexibility to swiftly and confidently shift their research to fight COVID-19 as well as future diseases and pandemics. “This is our career, the thing we’re passionate about,” Klimstra says of university researchers and their work. “We are here … even if people don’t realize it.”
 The sense of urgency is very real for Hodgson, who is on health care’s front lines. But before she saw her first COVID-19 patient, before most of the world was even aware of the pandemic, Dimitrov knew there was no time to waste.
The sense of urgency is very real for Hodgson, who is on health care’s front lines. But before she saw her first COVID-19 patient, before most of the world was even aware of the pandemic, Dimitrov knew there was no time to waste.
By January 10, 2020, once the novel virus’s genome was published online, Dimitrov had all of the information he needed to switch his lab’s research gears from cancer treatments to the ominous new virus.
A professor of medicine in the Division of Infectious Diseases and director of Pitt’s Center for Antibody Therapeutics, Dimitrov was no stranger to global viral contagions: In 2002 and 2012, with the emergence of the severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS) viruses, respectively, Dimitrov developed rapid methods of pinpointing the most potent human antibodies to fight novel, and sometimes fatal, coronaviruses.
“Scientifically, there was no difference [in SARS-CoV-2] from previous viruses in terms of what we were doing—making antibodies,” he says.
For the greatest chance of finding the most potent antibodies, it was important for Dimitrov and his team to have the largest possible pool of antibodies from which to hunt. For the past several years, he and his team have compiled about 1 trillion human antibodies, taken from the blood plasma of several hundred individuals, to create 10 libraries from which they would search for antibodies with the ability to neutralize the SARS-CoV-2 virus.
 They also knew, based on experience with SARS, that the composition of spike proteins—which protrude from the outside of coronaviruses—play a critical role in the virus’s infection of a cell. So, using the publicly available genome, team members Chuan Chen, a postdoctoral researcher, and Wei Li, an assistant professor in the Division of Infectious Diseases and assistant director of the Center for Antibody Therapeutics, created a supply of identical spike protein “keys” that the SARS-CoV-2 virus used to gain access to healthy cells.
They also knew, based on experience with SARS, that the composition of spike proteins—which protrude from the outside of coronaviruses—play a critical role in the virus’s infection of a cell. So, using the publicly available genome, team members Chuan Chen, a postdoctoral researcher, and Wei Li, an assistant professor in the Division of Infectious Diseases and assistant director of the Center for Antibody Therapeutics, created a supply of identical spike protein “keys” that the SARS-CoV-2 virus used to gain access to healthy cells.
Mixing the protein “keys” with each library, Li then used the keys as bait to lure and bind to the antibodies with the best fit—like dangling a key to “fish” for a corresponding lock.
“Once you isolate the antibody molecule,” Dimitrov says, “you can sequence its DNA and … do everything.” They don’t need to wait for infected individuals to provide antibodies via convalescent plasma. Thanks to their finely tuned method—what Dimitrov describes as the fastest possible way to isolate antibodies against a new pathogen—his team identified the world’s first human monoclonal antibodies (cloned from only one antibody) against SARS-CoV-2 in February 2020: namely, Ab1, a fully human antibody; and Ab8, consisting of a human antibody’s smallest molecular component.
The Ab1 and Ab8 results, published in Proceedings of the National Academy of Sciences and in Cell, respectively, show they were highly effective in preventing and treating COVID-19 in animal models.
In partnership with John Mellors, Pitt’s chief of the Division of Infectious Diseases and a professor of medicine and of infectious diseases and microbiology, Dimitrov cofounded Abound Bio—a UPMC-backed company that has licensed both antibody treatments for worldwide development—and is preparing for clinical trials.
If all goes well, he believes Ab1 and Ab8 could be approved by the U.S. Food and Drug Administration (FDA) for clinical use and available this year to treat COVID-19 patients like those Hodgson sees every night.
 With a global pandemic on Hodgson’s and the rest of the world’s shoulders, Dimitrov wasn’t the only one to quickly change research tracks in order to help fight COVID-19.
With a global pandemic on Hodgson’s and the rest of the world’s shoulders, Dimitrov wasn’t the only one to quickly change research tracks in order to help fight COVID-19.
As experts in “how viruses cause disease in animals and adding a therapeutic to that mix,” Klimstra and his colleagues were particularly equipped to handle the challenge: They are affiliated with Pitt’s Center for Vaccine Research (CVR), a multidisciplinary community of scientists interested in infectious disease. It boasts the expertise and infrastructure required for clinical trials and basic science—including the University’s Regional Biocontainment Laboratory, one of 14 distinct regional biocontainment laboratories established across the country by the National Institutes of Health. All this provides researchers like Klimstra with the resources needed to safely work with highly infectious, potentially dangerous pathogens.
Owing, in part, to his previous efforts working on the MERS coronavirus, Klimstra is helping develop another new antibody treatment for COVID-19 for the South Dakota-based biopharmaceutical company SAB Biotherapeutics. Through these efforts, he’s had to depend on some unusual colleagues: genetically modified dairy cows that possess a small amount of artificial human DNA.
 When the cows are given a piece of the SARS-CoV-2 virus, their human DNA controls the production of human antibodies that target SARS-CoV-2. (Don’t worry; the cows can still produce the bovine antibodies they need to protect themselves.) To create the drug, called SAB-185, scientists separate the human antibodies from the bovine ones.
When the cows are given a piece of the SARS-CoV-2 virus, their human DNA controls the production of human antibodies that target SARS-CoV-2. (Don’t worry; the cows can still produce the bovine antibodies they need to protect themselves.) To create the drug, called SAB-185, scientists separate the human antibodies from the bovine ones.
“When you’re given antibodies from another species, you mount an immune response to those,” Klimstra explains. “But when you’re given antibodies from humans, you actually mount a very small to negligible immune response”—which means individual patients could potentially be treated with SAB-185 multiple times in high doses. Also, he says, unlike monoclonal antibodies, the drug consists of many different types of antibodies that fight various parts of the virus.
But why cows? For one thing, compared to humans, they’re bigger and have more blood, therefore producing a larger supply. Additionally, their blood is naturally twice as antibody rich than that of humans. Both of these characteristics, says Klimstra, make these genetically modified cows, living on a South Dakota farm, superb antibody-producing “bioreactors.”
With the support of the Department of Defense and the National Institutes of Health, Klimstra is leading the analysis of SAB-185’s potency against SARS-CoV-2—shepherding it, if all goes well in the months ahead, from the test tube to clinical trials to emergency use authorization from the FDA. So far, the cow’s human antibodies have been an impressive four times more effective at preventing the coronavirus from entering healthy cells than the antibodies in human convalescent plasma, which may prove critical in controlling new viral strains.
With a phase I safety trial for SAB-185 now complete, Klimstra expects clinical trials to begin soon.
 While Klimstra’s bovine bioreactors enjoyed life on the farm, Shi, an assistant professor in Pitt’s Department of Cell Biology, and his lab teamed up with a different unlikely collaborator: a fluffy, black-haired llama named Wally.
While Klimstra’s bovine bioreactors enjoyed life on the farm, Shi, an assistant professor in Pitt’s Department of Cell Biology, and his lab teamed up with a different unlikely collaborator: a fluffy, black-haired llama named Wally.
Shi’s team depended on Wally’s ability to produce what are known as nanobodies, antibody fragments only produced in camelids—such as llamas, alpacas and camels—and in sharks. Although considerably smaller than full-sized human antibodies, nanobodies also bind to distinct pathogens in order to neutralize them and consequently protect healthy cells.
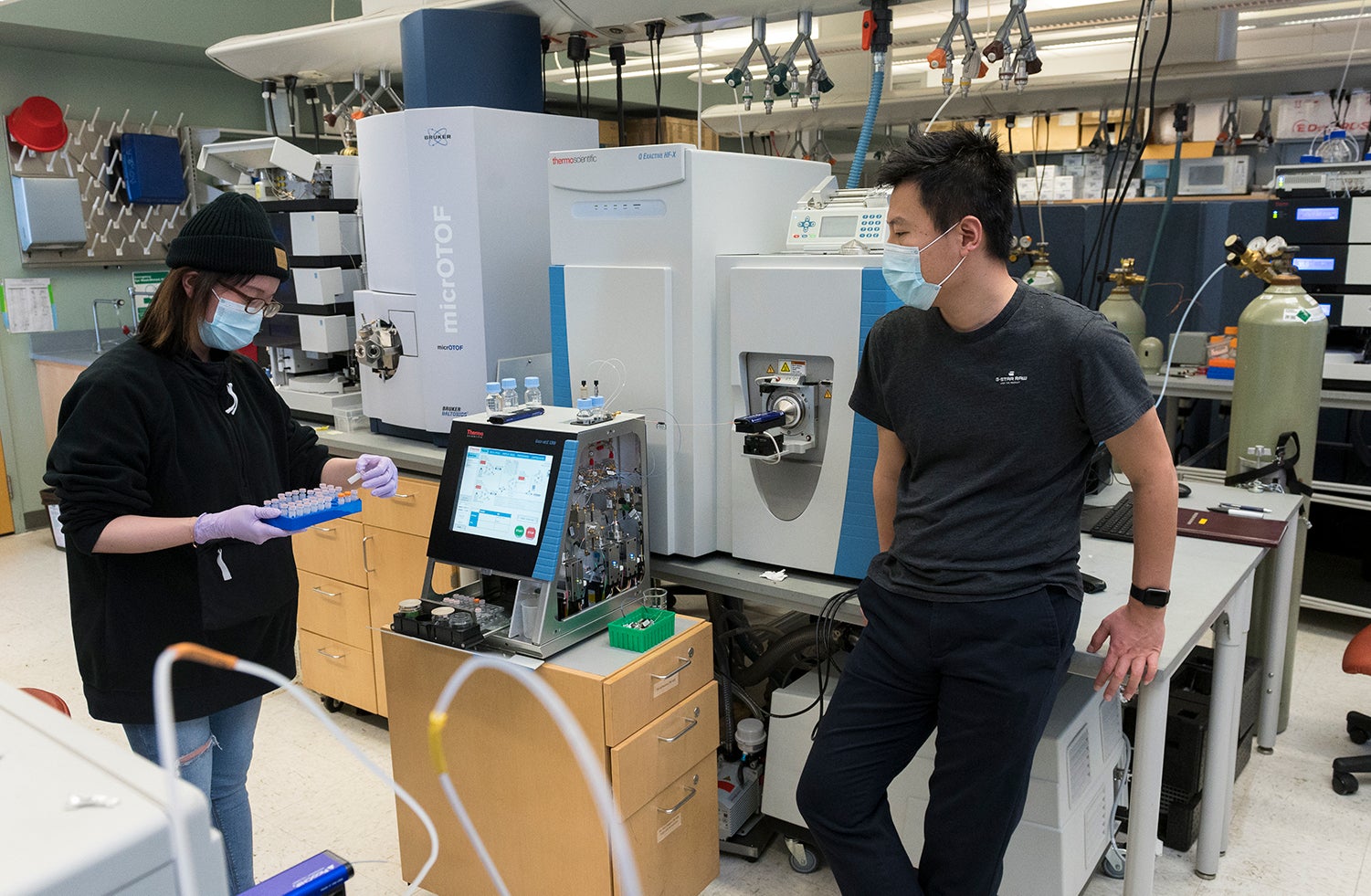
The challenge, according to Shi, is identifying “drug-quality” nanobodies—in other words, finding their amino acid sequences—for specific disease targets. A self-described “biochemist … trying to develop tools and technologies to analyze proteins and their molecular structures,” Shi believes that in order to find the best nanobodies for a specific disease target, scientists need something more than what the decades-old technology provides.
So, for the past three years, Shi and his lab of three researchers have “kind of buried ourselves in the sand,” Shi says, forgoing other projects in order to develop breakthrough technology and methods of identifying and producing top-quality nanobodies for any disease target of interest. “We struggled, we brainstormed, we talked with each other on an almost daily basis,” he says.
 It was, he adds, a “very high-risk project.” Thoroughly developing a new technology takes time—in their case, years of incremental progress that flies under the radar. “But we knew exactly what we were trying to do,” he says. “We saw the light at the end of the tunnel.”
It was, he adds, a “very high-risk project.” Thoroughly developing a new technology takes time—in their case, years of incremental progress that flies under the radar. “But we knew exactly what we were trying to do,” he says. “We saw the light at the end of the tunnel.”
Last spring, the pandemic gave Shi’s team an opportunity to pivot disease targets from cancer and Alzheimer’s disease to the new viral contagion: They decided to use their technology to identify drug-quality nanobodies that they could humanize (make more human) and use to effectively neutralize SARS-CoV-2.
To do this, they needed Wally’s help. By then, they had already been working with Wally, a resident of a Massachusetts farm, for two years. In coordination with Wally’s caretakers, who ensure his health and safety, Shi’s team had Wally immunized against the virus, enabling him to produce SARS-CoV-2-specific nanobodies after two months. Using the technology to analyze a small sample of Wally’s blood, lab member and research associate Yufei Xiang discovered thousands of nanobodies that, with help from colleagues in the CVR, were found to have unprecedented potency against the coronavirus. (And, Shi says, thanks to their technology and the many nanobodies it identified, the more likely it is that their drug could effectively neutralize viral variants.)
Published in Science and Cell Systems, their findings can potentially be used to develop inhalable therapeutics—a cheaper, easier and more direct means of treating the respiratory system than an IV—and, in turn, hopefully save lives.
The research of Shi, Klimstra, Dimitrov and their teams—along with the current vaccines in use and the other research being conducted by scientists worldwide—offers all of us hope in the midst of the pandemic.
Hope is what we need—more than 500,000 Americans and more than two million people worldwide have died as a result of COVID-19. Hodgson still remembers her patient, Jane, whom she left at the end of her shift in March 2020, wondering whether she’d survive the next 12 hours.
She did. But when Hodgson returned, Jane’s face, which the night before burned with the flush of fever, had since lost its color; her oxygen had declined to dangerously low levels. “She just looked like she wasn’t there anymore,” Hodgson recalls.
So, Hodgson whispered the same words to Jane that she had uttered to her gravely ill grandmother a few years before: “It’s okay to go.”
A short time later, she was gone.
In the year since Jane’s death, Hodgson has carried on, doing her part to bring some light to this pandemic darkness—as have Pitt researchers and so many others.
This article appears in the Spring 2021 edition of Pitt Magazine.